Surgeon or Software? Inside the Operating Room Where Robots Call the Shots
Key Takeaways: The State of AI Surgery in 2026
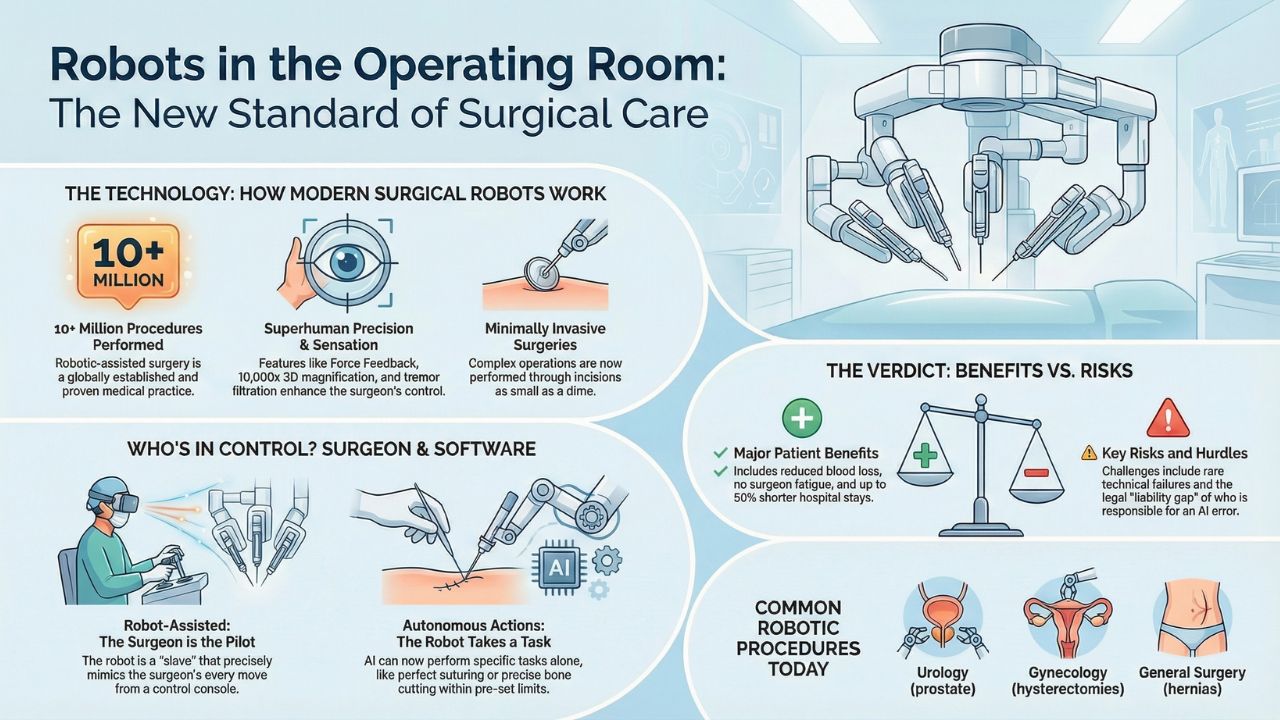
- It is not Sci-Fi: Over 10 million robotic-assisted procedures have already been performed globally.
- The Da Vinci 5 Era: New systems now feature Force Feedback, allowing surgeons to "feel" tissue remotely.
- Autonomy Levels: Most robots are still puppets controlled by doctors, but fully autonomous suturing is now a reality.
- Safety Stats: Robotic surgery reduces hospital stays by 50% in complex cases, though initial costs remain high.
The Silent Revolution in the O.R.
Imagine lying on the operating table. The lights are bright, the anesthesia is kicking in, and you look up to see your surgeon.
But instead of a human in a mask, you see a massive, four-armed machine looming over you.
This isn't a dystopian movie; it is the reality of modern healthcare.
We are witnessing the shift from human hands to autonomous robotic surgery.
This article investigates specifically how reliable these machines are and whether we are ready to let software hold the scalpel.
Note: This investigation is a critical chapter of our extensive guide on the Clinical AI MedTech Revolution: How Algorithms Are Saving Lives.
Da Vinci 5 & The New Standard of Precision
When we talk about the future of surgical robotics, we are usually talking about one dominant player: Intuitive Surgical’s Da Vinci systems.
In 2026, the Da Vinci 5 is the gold standard. But it is not just a fancy tool;
it is a data-processing powerhouse.
Unlike previous versions, the modern Da Vinci 5 AI features include:
- Haptic Feedback: Surgeons sitting at the console can now "feel" the resistance of tissue, preventing accidental tears.
- Tremor Filtration: The AI automatically cancels out any shaking in the surgeon's hand, allowing for micron-level precision.
- 10,000x Magnification: 3D visualization that human eyes simply cannot match.
Result:
Surgeries that used to require huge incisions now happen through holes the size of a dime.
Assisted vs. Autonomous: Who is Actually Cutting?
This is the most common question patients have: "Is the robot thinking for itself?"
Currently, the answer is usually "No, but..."
We categorize surgical AI into two buckets:
1.Robot-Assisted Surgery (The Current Standard) The robot is a "Slave."
It does nothing unless the human surgeon moves their hands at the console.
The AI is there to smooth out movements and improve vision.
2. Autonomous Robotic Surgery (The Emerging Frontier) This is where AI in surgery pros and cons get debated.
In 2026, we are seeing robots perform specific tasks without human intervention, such as:
- Smart Suturing: Stitching up a wound with perfect, mathematical spacing.
- Bone Cutting: In orthopedic knee replacements, the robot cuts bone within a pre-planned boundary and stops automatically if it gets too close to a nerve.
The Safety Question: Human Error vs. Machine Glitch
Is robot-assisted surgery safety superior to human hands?
The data suggests Yes, but with caveats.
The Pros:
- Reduced Blood Loss: Precise cauterization means less bleeding.
- Faster Recovery: Patients often go home in 24 hours rather than 5 days.
- No Fatigue: A robot does not get tired after a 12-hour heart transplant.
The Cons (The Risks):
- Latency Issues: A millisecond delay in the video feed can be catastrophic.
- Technical Failure: Systems can freeze (though extremely rare).
- The Liability Gap: This is the biggest hurdle.
If a human doctor slips, it is malpractice. But if the robot makes a mistake, who is liable?
Is it the hospital, the surgeon, or the software developer?
We explore this legal nightmare and the fight for your rights in our deep dive on The Algorithm Denied My Surgery: AI Medical Ethics & Privacy Risks.
What Surgeries Are Robots Doing Today?
You might be surprised to learn which procedures are already dominated by bots.
If you are going in for any of the following, there is a high chance a robot will be involved:
- Urology: Radical prostatectomies (removal of the prostate) are 90% robotic in top US hospitals.
- Gynecology: Hysterectomies and fibroid removals.
- General Surgery: Hernia repairs and bariatric (weight loss) gastric bypasses.
- Thoracic: Lung biopsies where the robot navigates deep into the bronchial tubes.
Conclusion: The Surgeon of Tomorrow is a Pilot
The era of the "God Complex" surgeon standing alone is ending.
The surgeon of 2026 is more like a pilot. They monitor the instruments, set the course, and let the autonomous robotic surgery systems handle the turbulence.
It is safer, cleaner, and faster. But as we hand over more control to the machines, we must ensure we never lose the human judgment that saves lives when the code fails.
Frequently Asked Questions (FAQ)
While theoretically possible, surgical systems are usually air-gapped (not connected to the open internet) to prevent this specific nightmare scenario.
Yes. The equipment is expensive. However, insurance often covers it because the shorter hospital stay actually saves money in the long run.
Absolutely. You always have the right to informed consent. However, for procedures like prostate cancer, the robot's precision is statistically superior to open surgery.